MHC works with agencies to support implementation, review and design their research programs/strategies. If you need help with this, or any other related service, please get in touch.
The success of translating research into policy and practice hinges on planning an “implementation handover” from the start. This approach has proven effective in driving meaningful changes, as evidenced by the high implementation rate of projects funded under the NSW Health’s Translation Research grant scheme.
Plan an ‘implementation handover’ at the outset of any project so the ‘implementation team’ is ready to run with the findings to drive change. This tip could also apply to the innovations in pilot projects being implemented into business as usual.
We need to start talking about an ‘implementation handover’.
In really good news for evidence informed policy and practice, a recent review we conducted of an innovative research funding scheme in NSW showed its success in driving policy and practice changes.
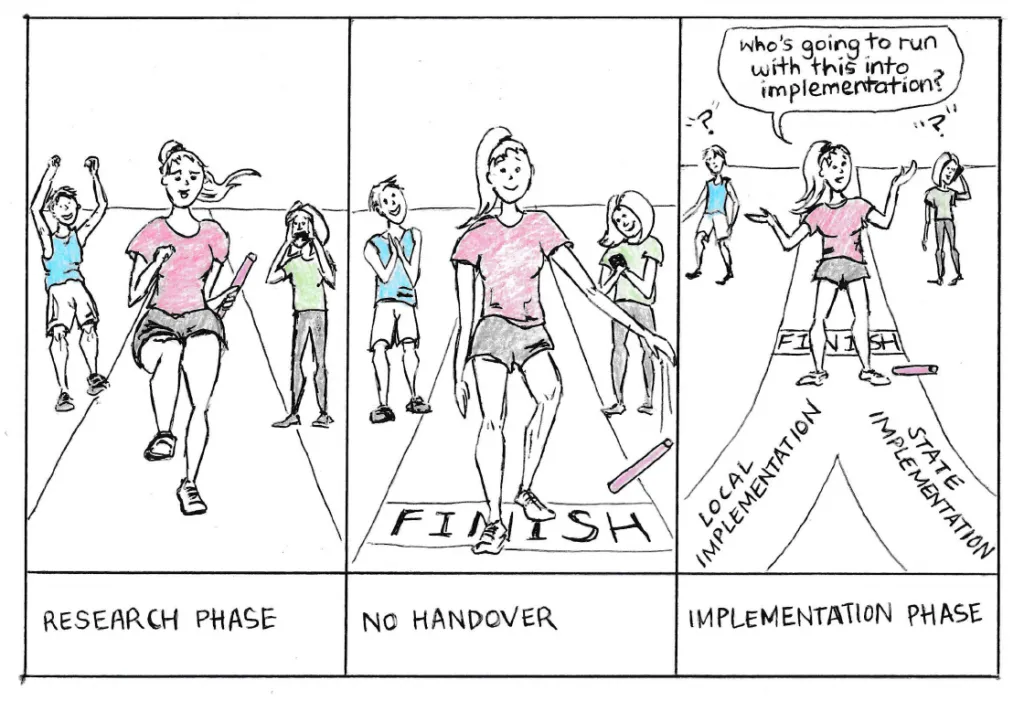
For decades now, across many sectors, we have puzzled over how to close the research-implementation gap, sometimes called the ‘know-do gap’. A common scenario is that important research is completed, the findings are reported and maybe even published, but never go any further… and end up in the ‘graveyard of good ideas’.
 Implementation by osmosis: a path to the graveyard of good ideas
Implementation by osmosis: a path to the graveyard of good ideasThere has been a vast improvement in ‘co-producing’ research, whereby researchers and practitioners partner together to ensure research is driven by practicality and need – in fact it is now a requirement of many research grants. This is akin to the notion of ‘co-design’ of programs and services.
But even with ‘co-production’ between researcher and practitioners the research-implementation gap still exists. In 2015, research looking at 50 federally funded intervention studies found that only 34% resulted in specific policy and practice changes.
So what to do when the research ends? Without a clear plan of who will consider the results – and, if relevant, act on them – we end up with an expectation of (or maybe hope for) ‘implementation by osmosis’.
But ideas don’t just magically swing into action, no matter how excellent. ‘Implementation by osmosis’ is a swift path to the graveyard of good ideas.
In 2016 NSW Health, through the Office for Health and Medical Research (OHMR), launched the Translation Research grant scheme. The scheme funds research that is conducted in the health system and is directly translatable into policy and practice, which will lead to improved health outcomes for the NSW population.
This scheme supports research that:
Importantly, research projects supported by this scheme have gained agreement from NSW Health CEOs to implement any relevant findings as part of the proposal process.
This is a distinctive and unique feature of this scheme compared with others.
The first tranche of projects funded in 2016 were finishing up in late 2018 and early 2019.
It was time to consider whether the completed projects funded under it were on track to be implemented in the NSW Health system.
Basically, to find out: was the scheme working?
To answer this question, NSW Health engaged MHC to assist with conducting an implementation review.
This involved reviewing documentation and interviewing the researchers and stakeholders from 10 projects from the first round, which was a pleasure. The investigators were a passionate group of people who could speak for hours about their project and health service.
We found that all projects were committed to the ongoing implementation of their findings into the system.
The challenge in a few instances was how to move it from a good idea into routine system operations. That transition required other players to become involved in the implementation.
Impressively, 7 out of the 10 (an outstanding 70%) had already resulted in changes to policy and practice – which everyone involved is really pleased with. (And a big difference from the 34% of federally funded research found in the 2015 review.)
Of course, not all findings from all research should be implemented. A range of factors must be considered: for example, the strength of the evidence and alignment with previous studies. Sometimes research suggests that an intervention does not benefit – or even can cause harm. In other cases implementation isn’t feasible due to high costs, or problems with acceptability in the community.
In this scheme, we found these were some of the factors that enabled implementation:
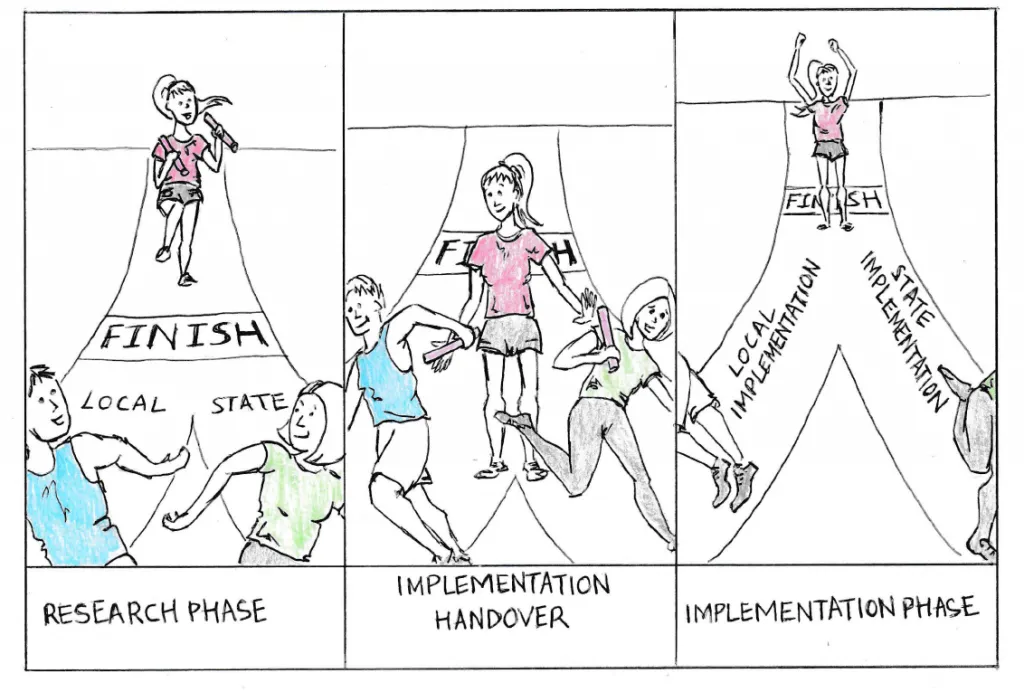
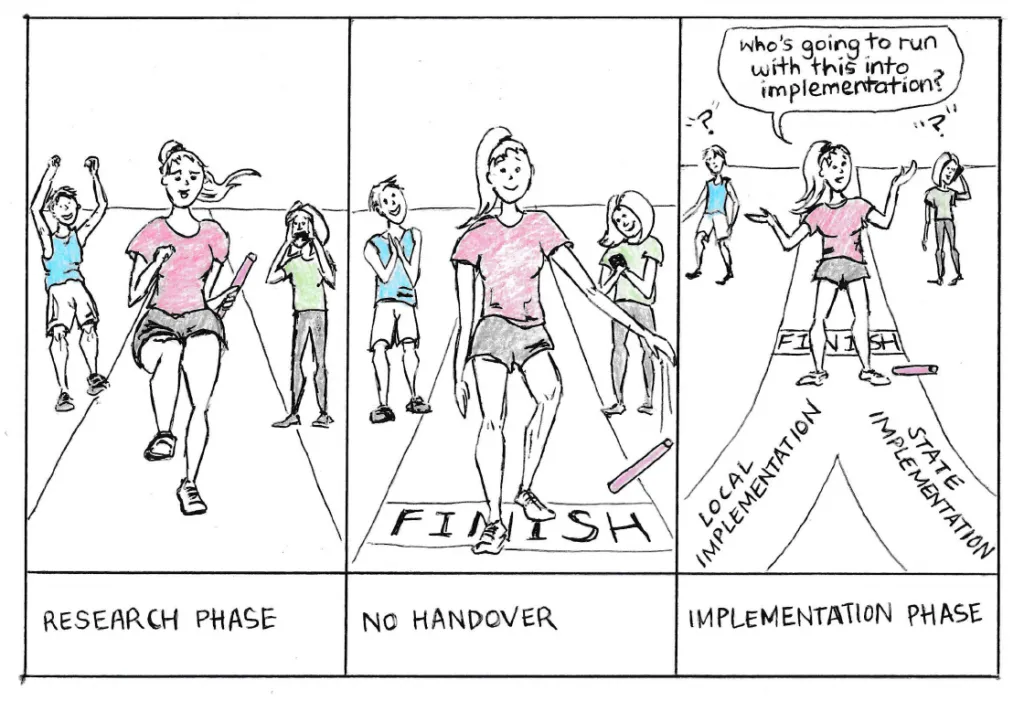
By far and away, having a planned implementation handover was the key feature of successful projects that we reviewed.
With a handover plan, we saw that as soon as the research finished, implementation was off to a flying start!
Based on this, the review recommended that all research projects under the scheme have a planned ‘implementation handover’ from the research team to local or statewide policy/practice partners to assess the intervention for implementation, and then to lead this process.
This handover needs to occur along an implementation pathway agreed to at the outset of research design. This implementation handover can even start while the research is still being completed if early findings are positive.
In an example of a hypothetical implementation pathway, a project could test whether home based telephone or computer based rehabilitation was better for patients than outpatient rehabilitation for a chronic condition.
The teams involved would be proud of this outcome, as they should be!
We need more research like this that ends up being rapidly implemented into our systems to benefit the communities we serve.
Our review tells us that this can be achieved by commissioning research differently and supporting an implementation hand over.
Acknowledgements: Graphics used in this post are copyright NSW Health.
© 2015-2025 MH Consulting Group (MHC) | Disclaimer | Privacy
